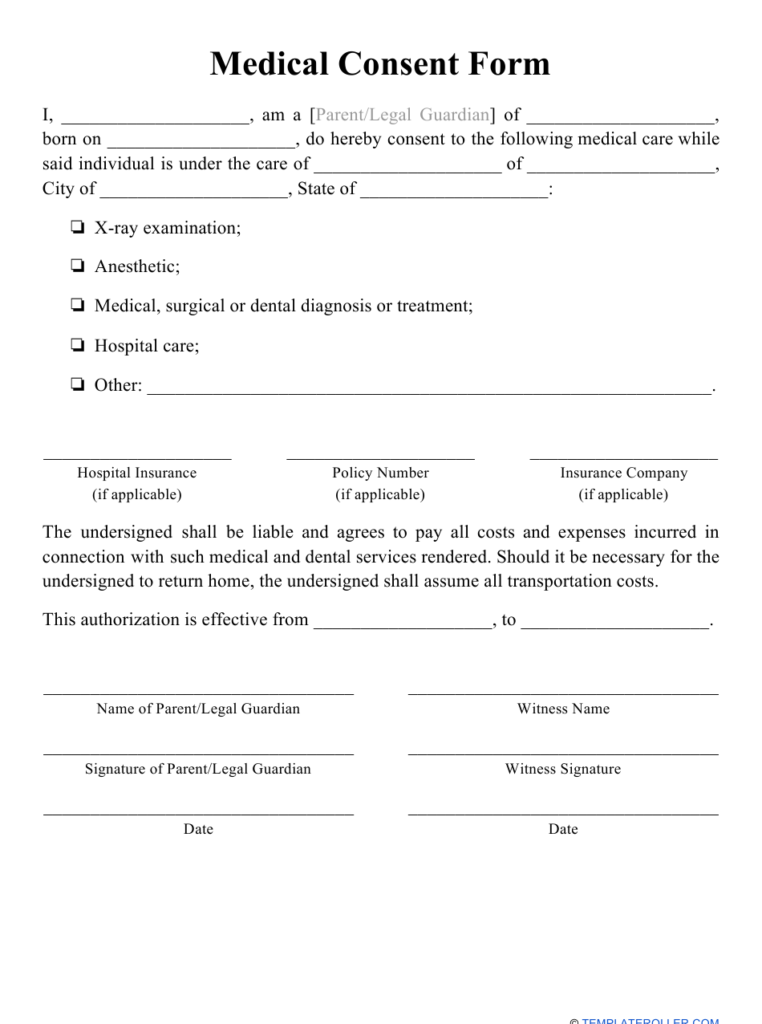
Consent Form Requirements – Everyone should be able to make informed choices about their medical care. Medical treatments can be quite demanding, and therefore patients should be able, in the end, to decide, based on known risks as well as their own personal preferences, how they will be treated. Thus, before medical professionals are allowed to provide treatment to patients they must be given the process of informed consent.
Informed consent constitutes a lawful requirement that requires that a patient be provided with a full and complete description of his or her physical state and the treatment recommended by the physician in charge. Once this information is received patients must offer the physician consent to treat before any form of care is administered. Without the patient’s informed consent the health professional cannot offer treatments.
Decision Making Capacity
In certain situations patients don’t have the capabilities to fully understand their treatment options and the risks/benefits associated with each. In other situations, patients may not be able to effectively convey their preferences to health workers. If this happens it is believed that the patient not to have adequate capacity for decision-making. If a family member is not present, or court-appointed representative in this case, can perform informed consent instead.
Patients who are strongly affected by their emotions – anxiety or fear, for example could be classified as lacking the ability to make decisions. The patients who are unconscious cannot make decisions on alone, and external parties are required to obtain consent instead.
Items in an Consent Form Requirements
Certain elements are commonly included in informed consent forms:
The patient’s medical condition/diagnosis
The procedure recommended by the physician in charge
The risks and the benefits associated with this procedure
Alternative treatments are available, along with their potential risks and benefits
The risks and benefits that come with refusing any treatment whatsoever
Not only must these items be documented in a written document, but they must also communicated with the person receiving the treatment. So, he is able to fully comprehend the details of the situation and receive direct responses to any questions that be arising.