Written Consent Forms Should Not Include – Everybody should be able to make informed choices about their health. Treatments for medical conditions can be demanding, and therefore patients should be able to determine from the facts about risks that their bodies should be treated. Thus, before medical professionals can administer treatments to patients, they must obtain the process of informed consent.
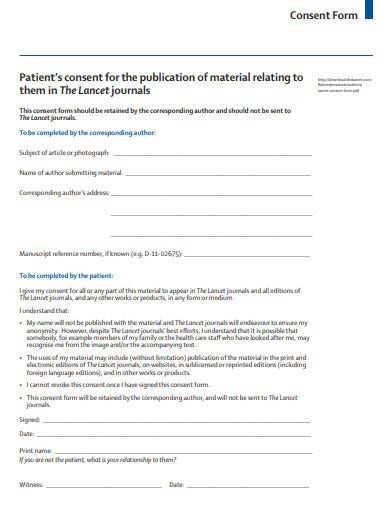
Informed consent constitutes a lawful requirement where a patient is provided with specific information regarding his or her physical health and the treatment recommended by the physician who is acting as the patient’s physician. After receiving this information patients must sign a consent form with the doctor to treat prior to any form of treatment can be provided. Without informed consent from the patient the health professional is not permitted to offer treatments.
Decision Making Capacity
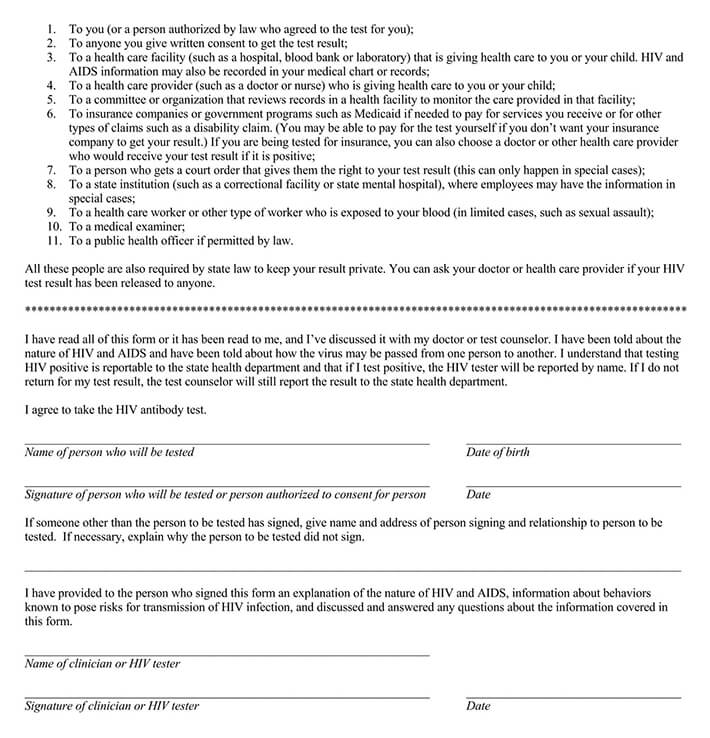
In some instances patients don’t have the skills to comprehend their options regarding treatment, and the risks/benefits of each one. In other situations patients may not be able explain their decisions to health professionals. If this happens, the patient is said not to possess the proper capacity for decision-making. If a family member is not present, or court appointed representative will then be permitted to perform informed consent instead.
Patients who are strongly affected by their emotions, like anxiety or fear, for example could be classified as not able to make decisions. The ones who are asleep clearly cannot take decisions on their own. Therefore, outside parties have to give consent for treatment instead.
Items in an Written Consent Forms Should Not Include
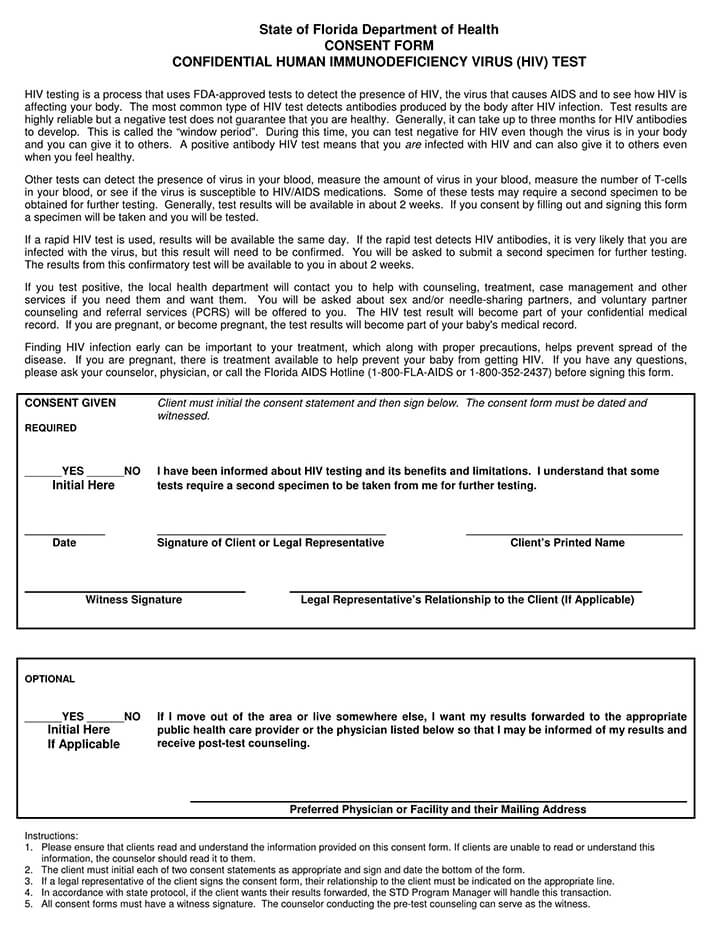
There are certain elements that are commonly included in informed consent forms:
The patient’s medical conditions/diagnosis
The treatment suggested by the medical professional in charge
The benefits and risks associated with this procedure
Alternative treatments are offered, as are their potential risks and benefits
The potential risks and rewards with refusing treatment at all
The items should not only be recorded in the patient’s medical records however, they must have a discussion with the patient. So, he is able to fully comprehend the specifics of the situation and will receive immediate responses to any issues that may have arisen.